Health conditions that affect soft tissues often develop quietly, revealing themselves only when discomfort or visible changes appear. One such condition that deserves careful attention is cellulogia, a term increasingly searched by patients looking for clarity about persistent skin inflammation and deeper tissue involvement. While it may sound unfamiliar, the experience behind it is not uncommon. Many people in the U.S. and UK encounter symptoms without immediately realizing their significance, delaying medical care that could prevent complications. This article takes a clear, human-centered approach to understanding cellulogia—how it begins, how it progresses, and when professional evaluation becomes essential. Drawing from medical insight, patient experience, and evidence-based guidance, the goal is to empower readers with knowledge rather than overwhelm them with jargon.
Table of Contents
ToggleWhat Is Cellulogia? A Clear Medical Overview
Cellulogia refers to an inflammatory condition involving the skin and underlying connective tissues, often linked to infection, immune response, or trauma. Unlike surface-level irritation, it penetrates deeper layers, which is why symptoms can escalate rapidly if untreated. Clinicians often categorize it alongside soft tissue infections, although its presentation can vary widely from person to person. In early stages, it may resemble a simple rash or localized swelling, leading many to underestimate its seriousness. Understanding this condition requires recognizing that it is not merely cosmetic or temporary; it represents an active physiological response that needs attention.
The Biological Story Behind Cellulogia
From a biological standpoint, cellulogia develops when bacteria or inflammatory agents breach the skin barrier. This can occur through minor cuts, insect bites, surgical wounds, or even microscopic cracks in dry skin. Once inside, the body’s immune system reacts by sending white blood cells to the area, triggering redness, warmth, and swelling. In some individuals, especially those with compromised immunity, the response can become exaggerated, spreading inflammation beyond the initial site. This internal narrative explains why early detection is crucial and why ignoring subtle changes can allow the condition to worsen.
Early Signs You Should Never Ignore
The earliest signs of cellulogia are often subtle but meaningful. Localized redness that expands over time, skin that feels warm to the touch, and tenderness are among the first indicators. Some patients report a tight or stretched sensation, while others notice mild pain that intensifies with pressure. These symptoms may be accompanied by fatigue or low-grade fever, signaling that the body is fighting something more than a surface irritation. Recognizing these early signals allows for timely intervention, often preventing the need for aggressive treatment later.
How Symptoms Progress Over Time
If left unaddressed, cellulogia can evolve quickly. Swelling may increase, the affected area can become firm, and pain often intensifies. In more advanced cases, blistering or skin dimpling may occur, and systemic symptoms such as chills or high fever can develop. This progression reflects the spread of inflammation through connective tissues and lymphatic pathways. Understanding this timeline helps patients appreciate why medical professionals emphasize early care rather than waiting for symptoms to “settle down.”
Risk Factors That Increase Susceptibility
Certain factors make individuals more prone to developing cellulogia. Chronic conditions such as diabetes, vascular disease, and autoimmune disorders can impair circulation and immune response, making infections harder to control. Lifestyle factors—like smoking, prolonged inactivity, or poor skin care—also play a role. Age is another consideration; older adults may experience thinner skin and slower healing, increasing vulnerability. Even athletes or active individuals are not immune, especially if repetitive friction or untreated minor injuries are involved.
How Doctors Diagnose Cellulogia
Diagnosis typically begins with a thorough clinical examination. Physicians assess the appearance, texture, and temperature of the affected area while reviewing medical history and recent skin injuries. In many cases, visual assessment is sufficient, but blood tests or imaging may be ordered if deeper infection is suspected. The goal is not only to confirm cellulogia but also to rule out similar conditions such as deep vein thrombosis or allergic reactions. Accurate diagnosis ensures that treatment is both targeted and effective.
Treatment Approaches and Medical Care
Treatment for cellulogia depends on severity and underlying cause. Mild cases often respond well to oral antibiotics, rest, and elevation of the affected limb. More advanced cases may require intravenous medication or short-term hospitalization. Alongside pharmaceutical treatment, doctors may recommend supportive measures such as hydration, proper wound care, and monitoring for changes. The emphasis is always on stopping the spread of inflammation while supporting the body’s natural healing process.
The Role of Lifestyle and Preventive Care
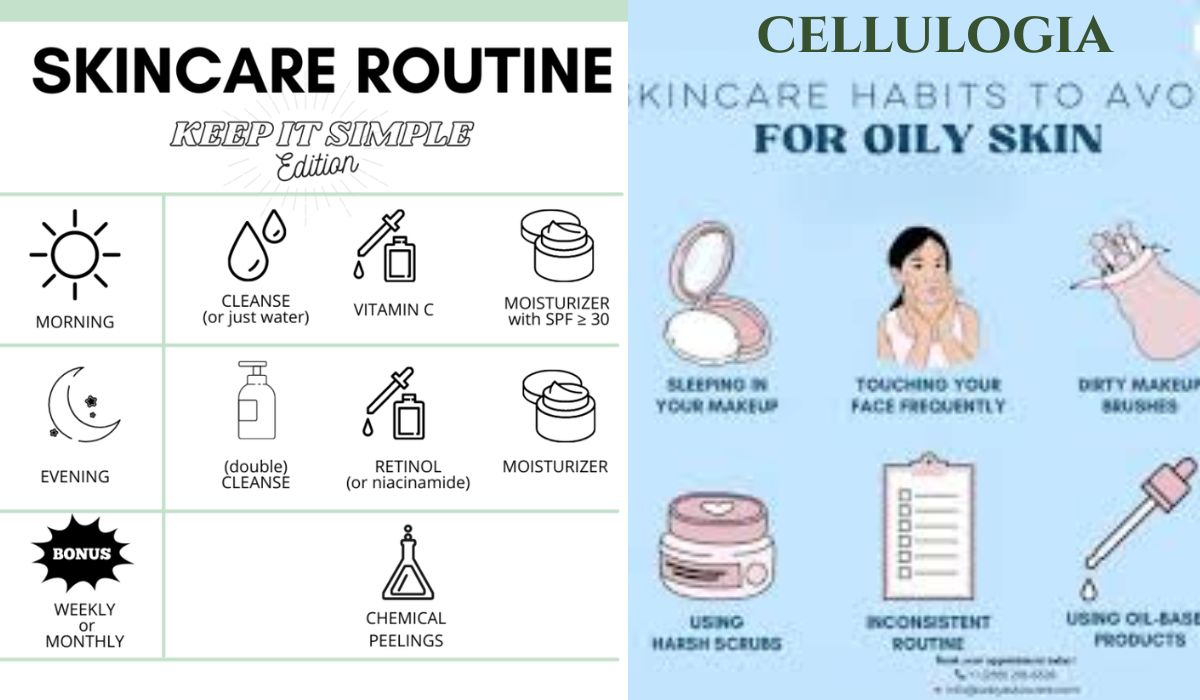
Preventing cellulogia involves consistent skin care and awareness. Keeping skin moisturized, promptly cleaning minor wounds, and avoiding prolonged pressure on vulnerable areas can significantly reduce risk. For individuals with chronic conditions, managing blood sugar levels and maintaining circulation through regular movement are particularly important. Preventive care also includes recognizing personal patterns—some people experience recurrent episodes, making vigilance a key part of long-term health management.
When to See a Doctor Without Delay
One of the most critical aspects of managing cellulogia is knowing when self-care is no longer enough. Rapidly spreading redness, increasing pain, fever, or numbness are all signs that professional evaluation is needed immediately. Delaying care can lead to complications such as abscess formation or systemic infection. Medical attention is not a sign of overreaction; it is a proactive step toward protecting overall health and preventing long-term damage.
Emotional and Psychological Impact
Beyond physical symptoms, cellulogia can take an emotional toll. Visible skin changes and recurring discomfort may affect confidence and daily functioning. Some patients experience anxiety, especially if episodes recur or interfere with work and social life. Addressing these concerns openly with healthcare providers can lead to more comprehensive care, including reassurance, education, and support strategies that acknowledge both physical and emotional well-being.
Long-Term Outlook and Recovery
With timely treatment, most individuals recover fully from cellulogia without lasting effects. Recovery time varies depending on severity, overall health, and how quickly treatment begins. Follow-up care is often recommended to ensure inflammation has resolved completely and to address any underlying risk factors. For those who experience recurrent episodes, long-term management plans can significantly reduce future risk, allowing patients to regain confidence in their health.
Conclusion
Understanding cellulogia is about more than recognizing a medical term; it’s about listening to your body and responding with informed action. Early signs are often subtle, but their implications are significant. By staying aware of risk factors, seeking timely care, and adopting preventive habits, individuals can protect themselves from complications and support long-term wellness. Knowledge, in this case, is not just power—it’s protection.
Frequently Asked Questions (FAQs)
1. Is cellulogia the same as cellulitis?
While cellulogia is often discussed alongside cellulitis, the terms are not always interchangeable. Cellulogia may be used to describe a broader inflammatory process involving connective tissue, whereas cellulitis is a well-defined bacterial skin infection. A healthcare provider can clarify the distinction based on symptoms and diagnostic findings.
2. Can cellulogia heal on its own without treatment?
Mild inflammation may appear to improve temporarily, but true cellulogia rarely resolves fully without medical care. Without proper treatment, symptoms can return or worsen. Early medical evaluation reduces the risk of complications and speeds recovery.
3. How long does recovery usually take?
Recovery time varies but often ranges from one to two weeks with appropriate treatment. More severe cases may require longer monitoring and follow-up. Adhering to prescribed care plans significantly improves outcomes.
4. Is cellulogia contagious?
No, cellulogia itself is not contagious. However, the bacteria that may contribute to the condition can spread through direct contact with open wounds. Practicing good hygiene and wound care minimizes any risk.
5. Can lifestyle changes reduce the risk of recurrence?
Yes, lifestyle adjustments play a meaningful role. Maintaining healthy skin, managing chronic conditions, staying active, and addressing minor injuries promptly can all reduce the likelihood of future episodes. Preventive care is especially important for those with a history of recurrence.
For More Update and Stories Visit: GOLDEN MAGAZINE